I am very privileged to have another guest post from a Physiotherapist that has just as much of an obsessive interest in Complex Regional Pain Syndrome as I do. Janet Holly (@innerchild) is a Senior Physiotherapist at Ottawa Hospital in Canada. Janet recently had a paper (ref) published with Tara Packham (@TaraLPackham) in the Journal of Hand Therapy entitled:
Mechanism-specific rehabilitation management of complex regional pain syndrome: Proposed recommendations from evidence synthesis.
I recently reached out to Janet to ask her for her experiences of working with people living with CRPS and to wright a short summary of her paper she wrote with Tara. So without further ado I will hand you over to Janet!
As a new grad many moons ago, there were a few diagnoses that could inspire internal terror in this newly minted clinician. CRPS or Reflex Sympathetic Dystrophy as it was known then, was one of them. In the early days of my career, treatment of CRPS seemed akin to torturing your patient. Yes, we did it in the best interest of our patient, but I always felt that the prescribed treatments did not address the human being who had CRPS. The treatments were targeting the traditional physiotherapy impairments of range of motion strength, gait, weightbearing etcetera and appeared to create intense suffering in some patients. If patient drop out rate was an indicator – it did. This was not what I signed up for in becoming a physiotherapist.
Nowadays, my practice involves a high percentage of CRPS patients and rather then wanting to run, I find the condition one that excites the critical thinking areas of my brain. Although much has been researched both on the neurophysiology, immunology and possible treatments of CRPS, there is much to learn yet. As it is a condition with a low prevalence rate it is difficult to conduct high powered studies to inform our practice (deMos et al., 2007).
In a discussion with Tara Packham, OT, in the fall of 2017, we determined that although the scientific literature had tailored pharmacological treatments based on the presenting mechanistic neurophysiology and immunology of the patient conservative treatments had yet to be truly structured around mechanism. The prevailing evidence-based rehabilitation treatment regimes were like throwing spaghetti at a wall to see what stuck.

As a result, we set out to do a systematic review of the rehabilitation literature in a mechanistic methodology. Using the work of Gierthmuhlen et al., (2014) as inspiration, eight different mechanisms were mapped out. These mechanisms were: targeting peripheral mechanism (inflammation, oxidative stress/hypoxia, allodynia/hyperalgesia) and targeting central mechanisms (body perception disturbance, learned non-use/pseudoneglect, neuroplasticity, kinesiophobia, psychological distress).
A systematic search of the literature was done which revealed 126 articles which reduced to 74 papers after abstract review. In the end, 49 papers were eligible for our review. (Packham & Holly, 2018) The final results revealed conservative management strategies linked to each of the eight mechanisms proposed by Gierthmuhlen (Gierthmuhlen, Binder, & Baron, 2014).
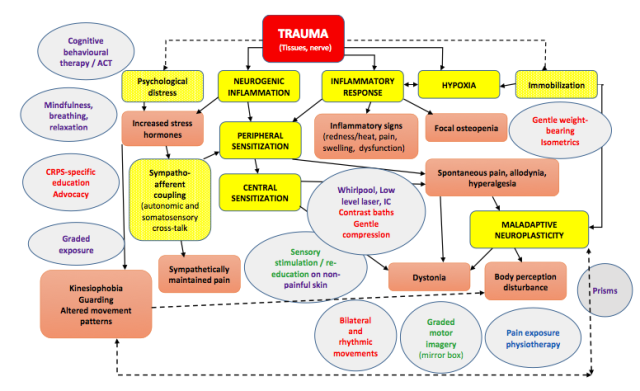
Evidence for the clear majority of treatments was poor with ratings ranging from 0 to 8/10 on the PEDro evidence scale. Even studies that obtained a high PEDro rating were found to have significant flaws when appropriately critically appraised. The length of this blog does not allow a detailed sharing of each treatment, but the diagram below summarizes the treatments found within the mechanism they address. The level of evidence for each treatment is colour coded. However, one treatment may address two different mechanisms. We stress that treating clinicians should not be solely focussed on impairments to drive their treatment strategies but rather take a dual top down approach of managing participation dysfunction and quality of life all the while addressing corresponding signs and symptoms that are unique to the individual patient’s CRPS experience from a bottom up methodology. This is in line with the World Health Association’s International Classification of Functioning, Disability and Health which emphasizes the need to restore participation in health interventions (World Health Organization, 2002).
Interventions such as splints or modified activities can be seen by some clinicians as enabling disability; however, clinicians should critically reflect on each individual case. The splint or modified activity may be allowing for greater participation in other life activities by avoiding a “flare” which last longer then an hour. In this case the splint could be allowing the continuation of important life roles such as engaging in a recreational activity with their children after school.
Key:
- High quality evidence
- Moderate quality evidence
- Preliminary evidence
- Expert opinion
Clinical practice guidelines in this population rely heavily on expert opinion. They emphasize a need for participation and activity-based therapy with constant grading to promote change. However, the literature which looked at occupational therapy treatments stressed (Lageux et al 2018, Rome et al 2016) the need to individualize the treatments for each patient. Their needs to be an emphasis of being mindful that some patients will push and exceed their activity baselines. This constant exceeding of baselines can lead to worsening of signs and symptoms with the result being significantly disrupted sleep secondary to pain. (page 4 of our review). In this population continuing to push a patient when pain is increasing and sleep is continuing to deteriorate can be risky. The literature informs us that the rate of suicidal ideation can be as great as 74% (Lee, et al., 2014) and continued sleep deprivation is associated with anxiety and depression (Finan et al., 2013; Schaefer et al., 2014).
Our review found a need for clinicians to start reflecting on their practice of relying on old treatments that are versed in expert opinion solely and considering some of the principles of pain neurophysiology. For example, rather then using contrast baths, perhaps the clinician should be introducing thermal sensory inputs in a graded progression of slowly decreasing the water temperature rather then immersion in very cold water. The same approach can be used with mechanical loading of a limb versus jumping into full loading. Treatments should be congruent with what we know about pain neurophysiology.
Our review found that evidence-based treatments that address vasomotor instability from stress hormones, sympathoafferent coupling, dystonia and focal osteopenia were still lacking. Research in these areas should be targeted. Emerging technologies may also bring promise of potential future treatments as our database searches uncovered some case reports using virtual reality. There is much to continue to explore and research in determining evidence-based treatments for CRPS as we learn more about its pathophysiological mechanisms.
This blog explored the literature specific to CRPS. However, we have learned much in the treatment of other pain conditions that informs us that our treatment strategies should not end there. The work of rehabilitation professionals like Maxi Miciak, Folarin Babatunde and Paulo Ferreira informs us that establishing excellent patient specific therapeutic relationships is as important as the specific techniques we use. Rather then go into the specifics of their research, a light-hearted word search has been constructed that includes key features of therapeutic relationships and focussed patient goal setting.
ADVOCACY AVOCATION
CHEERLEAD CREATIVITY
EMPATHY GENTLENESS
JOY KINDNESS
LIFE MOBILITY
PACE PARTICIPATION
PARTNERSHIP PATIENCE
PEACE QOL
ROLES SAFETY
SLEEP TRUST
UNDERSTANDING VALIDATION
Thanks so much to Janet for her insights and synopsis of her research with Tara. CRPS is a debilitating condition and a challenging condition to manage, there is still much to learn. Advances are being made and at a steady pace that can only be encouraging for future treatments. Check out some of the other CRPS blogs under the CRPS link in the categories section.
Thanks again for having a read
TNP
References:
- de Mos M, de Bruijn GJ, Huygen FJPM, Dieleman JP, Stricker BHC, Sturkenboom MCJM. The incidence of complex regional pain syndrome: A population-based study. Pain. 2007;129(1-2):12-20. doi:10.1016/j.pain.2006.09.008.
- Packham, T., & Holly, J. (2018, February 13). Mechanism-specific rehabilitation management of complex regional pain syndrome: Proposed recommendatons from evidence synthesis. Journal of Hand Therapy. doi:10.1016/j.ht.2018.01.007Packham, T., & Holly, J. (2018, February 13). Mechanism-specific rehabilitation management of complex regional pain syndrome: Proposed recommendatons from evidence synthesis. Journal of Hand Therapy. doi:10.1016/j.ht.2018.01.007
- Harden RN, Oaklander AL, Burton AW, et al. Complex regional pain syndrome: practical diagnostic and treatment guidelines. Pain Med. 2013;14:180-229. doi:10.1111/pme.12033.
- Borchers AT, Gershwin ME. Complex regional pain syndrome: A comprehensive and critical review. Autoimmun Rev. 2014;13(3):242-265. doi:10.1016/j.autrev.2013.10.006.
- Stanton-Hicks M. Complex regional pain syndrome. Anesthesiol Clin North America. 2003;21(4):733-744. doi:10.1016/S0889-8537(03)00084-1.
- Wasner G, Schattschneider J, Binder a, Baron R. Complex regional pain syndrome–diagnostic, mechanisms, CNS involvement and therapy. Spinal cord. 2003;41(2):61-75. doi:10.1038/sj.sc.3101404.
- de Mos M, Sturkenboom MCJM, Huygen FJPM. Current understandings on complex regional pain syndrome. Pain Pract. 2009;9(2):86-99. doi:10.1111/j.1533-2500.2009.00262.x.
- Birklein F, O’Neill D, Schlereth T. Complex regional pain syndrome: An optimistic perspective. Neurology. 2015;84(1):89-96. doi:10.1212/WNL.0000000000001095.
- Turner-Stokes L, Goebel A. Complex regional pain syndrome in adults: concise guidance. Clin Med. 2011;11(6):596-600.
- Stanton-Hicks M, Baron R, Boas R, et al. Complex Regional Pain Syndromes: guidelines for therapy. Clin J Pain. 1998;14(2):155-166.
- Harden, Swan M, King A, Costa B, Barthel J. Treatment of complex regional pain syndrome: functional restoration.Clin J Pain. 2006;22(5):420-424.
- Perez RS, Zollinger PE, Dijkstra PU, et al. Evidence based guidelines for complex regional pain syndrome type 1. BMC Neurol. 2010;10:20. doi:10.1186/1471-2377-10-20.
- van Eijs F, Stanton-Hicks M, Van Zundert J, et al. Evidence-based interventional pain medicine. 16. Complex regional pain syndrome. Pain Pr. 2011;11(1):70-87. doi:10.1111/j.1533-2500.2010.00388.x.
- Werner GT, Beyer A, Berliner M, et al. Therapierichtlinie der deutschen gesellschaft für physikalische medizin und rehabilitation – Behandlung beim komplexen regionalen schmerzsyndrom (sympathische Reflexdystrophie). Phys Medizin Rehabil Kurortmedizin. 2002;12(4):208-210. doi:10.1055/s-2002-33900.
- Ezendam D, Bongers RM, Jannink MJA. Systematic review of the effectiveness of mirror therapy in upper extremity function. Disabil Rehabil. 2009;31(26):2135-2149.
- Cossins L, Okell RW, Cameron H, Simpson B, Poole HM, Goebel A. Treatment of complex regional pain syndrome in adults: A systematic review of randomized controlled trials published from June 2000 to February 2012. Eur J Pain (United Kingdom). 2013;17(2):158-173. doi:10.1002/j.1532-2149.2012.00217.x.
- O’Connell NE, Wand BM, McAuley J, Marston L, Moseley GL. Interventions for treating pain and disability in adults with complex regional pain syndrome‐an overview of systematic reviews. Cochrane Database Syst Rev. 2013;(4). doi:10.1002/14651858.CD009416.pub2.
- Galve-Villa M, Rittig-Rasmussen B, Mikkelsen LMS, Poulsen AG. Complex regional pain syndrome Complex regional pain syndrome. Man Ther. 2016. doi:10.1136/bmj.h2730.
- McCabe CS. 2013 McCabe evidence based vs trial and error. Pain Manag. 2013;3(2):147-155.
- Pertoldi S, Di Benedetto P. Shoulder-hand syndrome after stroke. A complex regional pain syndrome. Eura Medicophys. 2005;41(4):283-292.
- Roosink M, Renzenbrink GJ, Geurts ACH, Ijzerman MJ. Towards a mechanism-based view on post-stroke shoulder pain: Theoretical considerations and clinical implications. NeuroRehabilitation. 2012;30(2):153-165. doi:10.3233/NRE-2012-0739.
- Perez RSGM, Zollinger PE, Dijkstra PU, et al. Evidence based guidelines for complex regional pain syndrome type 1. BMC Neurol. 2010;10(20). doi.org/10.1186/1471-2377-10-20.
- Goebel A, Barker C, Turner-Stokes L, et al. Complex Regional Pain Syndrome in Adults: UK Guidelines for diagnosis , referral and management in primary and secondary care.London: RCP, 2012.
- Daly AE, Bialocerkowski AE. Does evidence support physiotherapy management of adult Complex Regional Pain Syndrome Type One? A systematic review. Eur J Pain. 2009;13(4):339-353. doi:10.1016/j.ejpain.2008.05.003.
- Smart KM, Wand BM, O’Connell NE. Physiotherapy for pain and disability in adults with complex regional pain syndrome (CRPS) types I and II. Cochrane Database Syst Rev. 2016;2016(2). doi:10.1002/14651858.CD010853.pub2.
- Rothgangel AS, Braun SM, Beurskens AJ, Seitz RJ, Wade DT. The clinical aspects of mirror therapy in rehabilitation: a systematic review ofthe literature. Int J Rehabil Res. 2011;34(1):1-13. doi:10.1097/MRR.0b013e3283441e98.
- Thieme H, Morkisch N, Rietz C, Dohle C, Borgetto B. The efficacy of movement representation techniques for treating limb pain – a systematic review and meta-analysis. J Pain. 2016;17(2):167-180. doi:10.1016/j.jpain.2015.10.015.
- Barnhoorn KJ, van de Meent H, van Dongen RTM, et al. Pain exposure physical therapy (PEPT) compared to conventional treatment in complex regional pain syndrome type 1: a randomised controlled trial. BMJ Open. 2015;5(12):e008283. doi:10.1136/bmjopen-2015-008283.
- Duman I, Ozdemir A, Tan AK, Dincer K. The efficacy of manual lymphatic drainage therapy in the management of limb edema secondary to reflex sympathetic dystrophy. Rheumatol Int. 2009;29(7):759-763. doi:10.1007/s00296-008-0767-5.
- Kocic M, Lazovic M, Dimitrijevic I, Mancic D, Stankovic A. Procena terapijskog efekta lasera male snage i interferentnih struja kod bolesnika sa kompleksnim regionalnim bolnim sindromom primenom infracrvene termovizijske kamere. Vojnosanit Pregl. 2010;67(9):755-760.
- Moseley GL. Graded motor imagery for pathologic pain: A randomized controlled trial. Neurology. 2006;67(12):2129-2134. doi:10.1212/01.wnl.0000249112.56935.32.
- Oerlemans HM, Oostendorp RA, de Boo T, Goris RJ. Pain and reduced mobility in complex regional pain syndrome I: outcome of a prospective randomised controlled clinical trial of adjuvant physical therapy versus occupational therapy. Pain. 1999;83(1):77-83.
- Lagueux É, Bernier M, Bourgault P, et al. The Effectiveness of Transcranial Direct Current Stimulation as an Add-on Modality to Graded Motor Imagery for Treatment of Complex Regional Pain Syndrome.; 2017. Clin J Pain June 16. doi:10.1097/AJP.0000000000000522. [E-pub ahead of print]
- Devrimsel G, Turkyilmaz AK, Y ildirim M, Beyaza MS. The effects of whirlpool bath and neuromuscular electrical stimulation on complex regional pain syndrome. J Phys Ther Sci. 2015; 27(1):30-33.
- Moseley GL. Graded motor imagery is effective for long-standing complex regional pain syndrome: A randomised controlled trial. Pain. 2004;108(1-2):192-198.
- Moseley GL. Is successful rehabilitation of complex regional pain syndrome due to sustained attention to the affected limb? A randomised clinical trial. Pain. 2005;114(1-2):54-61. doi:10.1016/j.pain.2004.11.024.
- Korpan MI, Dezu Y, Schneider B, Leitha T, Fialka-Moser V. Acupuncture in the treatment of posttraumatic pain syndrome. Acta Orthop Belg. 1999;65(2):197-201.
- den Hollander M, Goossens M, de Jong J, et al. Expose or protect? A randomized controlled trial of exposure in vivo vs pain-contingent treatment as usual in patients with complex regional pain syndrome type 1. Pain. 2016;157(10):2318-2329. doi:10.1097/j.pain.0000000000000651.
- Ryan CG, King R, Robinson V, et al. Transcutaneous electrical nerve stimulation using an LTP-like repetitive stimulation protocol for patients with upper limb complex regional pain syndrome : A feasibility study. Hand Ther2017;22(2):1-12. doi:10.1177/1758998316678588.
- Moseley GL, Zalucki NM, Wiech K. Tactile discrimination , but not tactile stimulation alone , reduces chronic limb pain. J Pain; 2008;137:600-608. doi:10.1016/j.pain.2007.10.021.
- Moseley GL, Gallace A, Di Pietro F, Spence C, Iannetti GD. Limb-specific autonomic dysfunction in complex regional pain syndrome modulated by wearing prism glasses. Pain. 2013;154(11):2463-2468. doi:10.1016/j.pain.2013.07.026.
- McCabe CS. A controlled pilot study of the utility of mirror visual feedback in the treatment of complex regional pain syndrome (type 1). Rheumatology. 2003;42(1):97-101. doi:10.1093/rheumatology/keg041.
- Rome L. The place of occupational therapy in rehabilitation strategies of complex regional pain syndrome: Comparative study of 60 cases. Hand Surg Rehabil. 2016;35(5):355-362. doi:10.1016/j.hansur.2016.06.005.
- Gillespie S, Cowell F, Cheung G, Brown D. Can we reduce the incidence of complex regional pain syndrome type I in distal radius fractures? The Liverpool experience. Hand Ther. 2016;21(4):123-130. doi:10.1177/1758998316659676.
- Cho S, McCracken LM, Heiby EM, Moon DE, Lee JH. Pain acceptance-based coping in complex regional pain syndrome Type I: Daily relations with pain intensity, activity, and mood. J Behav Med. 2013;36(5):531-538. doi:10.1007/s10865-012-9448-7.
- Moseley GL, Wiech K. The effect of tactile discrimination training is enhanced when patients watch the reflected image of their unaffected limb during training. Pain. 2009;144(3):314-319. doi:10.1016/j.pain.2009.04.030.
- Packham TL, Spicher CJ, MacDermid JC, Michlovitz SL, Buckley DN. Somatosensory rehabilitation for allodynia in CRPS of the upper limb: a retrospective cohort study. J Hand Ther. 2017. doi:doi: 10.1016/j.jht.2017.02.007.
- Lagueux E, Charest J, Lefrançois-Caron E, et al. Modified graded motor imagery for complex regional pain syndrome type 1 of the upper extremity in the acute phase. Int J Rehabil Res. 2012;35(2):138-145. doi:10.1097/MRR.0b013e3283527d29.
- Johnson S, Hall J, Barnet S, et al. Using graded motor imagery for complex regional pain syndrome in clinical practice: Failure to improve pain. Eur J Pain. 2012;16(4):550-561. doi:10.1002/j.1532-2149.2011.00064.x.
- Christophe L, Chabanat E, Delporte L, et al. Prisms to Shift Pain Away: Pathophysiological and Therapeutic Exploration of CRPS with Prism Adaptation. Neural Plast. 2016;2016. doi:10.1155/2016/1694256.
- Schmid A-C, Schwarz A, Gustin SM, Greenspan JD, Hummel FC, Birbaumer N. Pain reduction due to novel sensory-motor training in Complex Regional Pain Syndrome I – A pilot study. Scand J Pain. 2017;15:30-37. doi:10.1016/j.sjpain.2016.11.003.
- Lewis JS, Kersten P, McPherson KM, et al. Wherever is my arm? Impaired upper limb position accuracy in Complex Regional Pain Syndrome. Pain. 2010;149(3):463-469. doi:10.1016/j.pain.2010.02.007.
- Selles RW, Schreuders T a R, Stam HJ. Mirror therapy in patients with causalgia (complex regional pain syndrome type II) following peripheral nerve injury: two cases. J Rehabil Med. 2008;40(4):312-314. doi:10.2340/16501977-0158.
- Grünert-Plüss N, Hufschmid U, Santschi L, Grünert J. Mirror therapy in hand rehabilitation: a review of, the literature, the st gallen protocol for mirror, therapy and evaluation of a case series of 52 patients. Br J Hand Ther. 2008;13(1):4-11. doi:10.1177/175899830801300101.
- Raucci U, Tomasello C, Marri M, Salzano M, Gasparini A, Conicella E. Scrambler Therapy(®) MC-5A for Complex Regional Pain Syndrome: Case Reports. Pain Pract. 2016;16(7):103-109. doi:10.1111/papr.12474.
- Mouraux D, Brassinne E, Sobczak S, et al. 3D augmented reality mirror visual feedback therapy applied to the treatment of persistent, unilateral upper extremity neuropathic pain: a preliminary study. J Man Manip Ther. 2017;25(3):137-143. doi:10.1080/10669817.2016.1176726.
- de Souza NS, Martins ACG, Bastos VH do V, et al. Motor imagery and its effect on complex regional pain syndrome: An integrative review. Neurol Int. 2015;7(3):58-61. doi:10.4081/ni.2015.5962.
- Smith TO. How effective is physiotherapy in the treatment of complex regional pain syndrome type I? A review of the literature. Musculoskeletal Care. 2005;3(4):181-200. doi:10.1002/msc.9.
- Dommerholt J. Complex regional pain syndrome — 2: physical therapy management. J Bodyw Mov Ther. 2004;8(4):241-248.
- McCabe C. Mirror visual feedback therapy. a practical approach. J Hand Ther. 2011;24(2):170-179. doi:10.1016/j.jht.2010.08.003.
- Pollard C. Physiotherapy management of complex regional pain syndrome. New Zeal J Physiother. 2013;41(2):65-72.
- Torta DM, Legrain V, Rossetti Y, Mouraux A. Prisms for pain. Can visuo-motor rehabilitation strategies alleviate chronic pain? Eur J Pain (United Kingdom). 2016;20(1):64-69. doi:10.1002/ejp.723.
- Lewis JS, Coales K, Hall J, McCabe CS. “Now you see it, now you do not”: sensory-motor re-education in complex regional pain syndrome. Hand Ther. 2011;16(2):29-38. doi:10.1258/ht.2011.011005.
- Lee D-H, Noh EC, Kim YC, et al. Risk Factors for Suicidal Ideation among Patients with Complex Regional Pain Syndrome. Psychiatry Investig. 2014;11(1):32. doi:10.4306/pi.2014.11.1.32.
- Watson HK, Carlson L. Treatment of reflex sympathetic dystrophy of the hand with an active “stress loading” program. J Hand Surg Am. 1987;12(5 Pt 1):779-785.
- Carlson L, Watson HK. Treatment of reflex sympathetic dystrophy using the stress-loading program. J Hand Ther. 1988;1:149-154.
- Finan PH, Goodin BR, Smith MT. The association of sleep and pain: An update and a path forward. J Pain. 2013;14(12):1539-1552. doi:10.1016/j.jpain.2013.08.007.
- Schaefer C, Mann R, Sadosky A, et al. Burden of illness associated with peripheral and central neuropathic pain among adults seeking treatment in the united states: A patient-centered evaluation. Pain Med (United States). 2014;15(12):2105-2119. doi:10.1111/pme.12502.
- Walsh MT, Muntzer E. Therapist’s management of complex regional pain syndrome (reflex sympathetic dystrophy). In: Mackin E, Callahan AD, Skirven TM, Schnieder L, Osterman AL, Hunter J, eds. Rehabilitation of the Hand and Upper Extremity. 5th ed. St. Louis, Missouri: Mosby; 2002:1707-1724.
- Moseley GL. A pain neuromatrix approach to patients with chronic pain. Man Ther. 2003;8(3):130-140. doi:10.1016/S1356-689X(03)00051-1.
- Bean DJ, Johnson MH, Heiss-Dunlop W, Kydd RR. Factors Associated with Disability and Sick Leave in Early Complex Regional Pain Syndrome Type-1. Clin J Pain. 2015;1336(7):1. doi:10.1097/AJP.0000000000000234.
- De Jong JR, Vlaeyen JWS, De Gelder JM, Patijn J. Pain-related fear, perceived harmfulness of activities, and functional limitations in complex regional pain syndrome type i. J Pain. 2011;12(12). doi:10.1016/j.jpain.2011.06.010.
- Spicher C, Quintal I, Vittaz M. Reeducation Sensitive Des Douleurs Neuropathiques. 3rd ed. Montpellier, France: Sauramps Medical; 2015.
- Breger Stanton DE, Lazaro R, MacDermid JC. A Systematic Review of the Effectiveness of Contrast Baths. J Hand Ther. 2009;22(1):57-70. doi:10.1016/j.jht.2008.08.001.
- Hall J, Swinkels A, Briddon J, McCabe CS. Does Aquatic Exercise Relieve Pain in Adults With Neurologic or Musculoskeletal Disease? A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Arch Phys Med Rehabil. 2008;89(5):873-883. doi:10.1016/j.apmr.2007.09.054.
- Wasner G, Schattschneider J, Heckmann K, Maier C, Baron R. Vascular abnormalities in reflex sympathetic dystrophy (CRPS I): mechanisms and diagnostic value. Brain. 2001;124(Pt 3):587-599. doi:10.1093/brain/124.3.587.
- Rodham K, McCabe C, Blake D. Seeking support: An interpretative phenomenological analysis of an Internet message board for people with Complex Regional Pain Syndrome. Psychol Health. 2009;24(6):619-634. doi:10.1080/08870440802563245.
- Rodham K, Gavin J, Coulson N, Watts L. Co-creation of information leaflets to meet the support needs of people living with complex regional pain syndrome (CRPS) through innovative use of wiki technology. Informatics Heal Soc Care. 2015;0(0):1-15. doi:10.3109/17538157.2015.1008491.
- Grieve S, Adams J, Mccabe C. “What I Really Needed Was the Truth”. Exploring the Information Needs of People with Complex Regional Pain Syndrome. Musculoskeletal Care. 2016;14(1):15-25. doi:10.1002/msc.1107.
- Eccleston, C., Fisher, E., Craig, L., Duggan, G. B., Rosser, B. A. and Keogh E. Psychological therapies (Internet-delivered) for the management of chronic pain in adults. Cochrane Database Syst Rev. 2014;(2). doi:10.1002/14651858. CD010152.
- McCracken LM, Keogh E. Acceptance, Mindfulness, and Values-Based Action May Counteract Fear and Avoidance of Emotions in Chronic Pain: An Analysis of Anxiety Sensitivity. J Pain. 2009;10(4):408-415. doi:10.1016/j.jpain.2008.09.015.
- Keefe FJ, Huling D a., Coggins MJ, et al. Virtual reality for persistent pain: A new direction for behavioral pain management. Pain. 2012;153(11):2163-2166. doi:10.1016/j.pain.2012.05.030.
- Wright G. Using virtual reality to augment perception, enhance sensorimotor adaptation, and change our minds. Front Hum Neurosci. 2014;8(56):1-6. doi:10.3389/fnsy.201400056.
- Fukumori S, Miyake K, Gofuku A, Sato K. Assessment of Motor Function in Complex Regional Pain Syndrome With Virtual Reality-based Mirror Visual Feedback: A Pilot Case Study. Neurosci Biomed Eng. 2016;4(1):43-49. doi:10.2174/2213385203666151102214311.
- Won A, Tataru C, CM C, et al. Two virtual reality pilot studies for the treatment of pediatric CRPS. Pain Med. 2015;16(8):1644-1647.
- Bultitude JH, Rafal RD. Derangement of body representation in complex regional pain syndrome : report of a case treated with mirror and prisms. 2010:409-418. doi:10.1007/s00221-009-2107-8.
- World Health Organization. (2002). Towards a Common Language for Functioning, Disability and Health: ICF. Retrieved from http://www.who.int/classifications/icf/en/
- Lee, D.-H., Noh, E. C., Kim, Y. C., Hwang, J. Y., Kim, S. N., & Jang, J. H. (2014). Risk factors for suicidal ideation among patients with Complex Regional Pain Syndrome. Psychiatry Investigations, 11, 32-38. doi:10.4306/pi.2014.11.1.32
- Miciak M, Gross DP, Joyce A. (2012)A review of the psychotherapeutic ‘common factors’ model and its application in physical therapy: the need to consider general effects in physical therapy practice. Scand J Caring sciences 26 (2), 394-403
- Fuentes J, Armijo-Olivo S, Funabashi M, Miciak M, Dick B, Warran S et al. (2014) Enhanced therapeutic alliance modulates pain intensity and muscle pain sensitivity in patients with chronic low back pain: an experimental controlled study.Physical therapy 94 (4), 477-489.
- Babatunde F, Macdermid JC, MacIntyre N. Characteristics of therapeutic alliance in musculoskeletal physiotherapy and occupational therapy practice: a scoping review of the literature. (2017) BMC Health Services Research 17(1). Doi:10.1186/s12913-017-2311-3
- Ferreira PH, Ferrera ML, Maher CG, Refshauge KM, Latimer J, Adams RD. (2013) The therapeutic alliance between clinicians and patients predicts outcome in chronic low back pain. Physical Therapy 93(4):470-478. https://doi.org/10.2522/ptj.20120137

